As the federal government shutdown extends into its second week, growing concerns are emerging over its immediate and far-reaching impact on health care providers who serve military families.
San Antonio, a city often referred to as “Military City USA,” finds itself at the epicenter of this crisis, given its significant concentration of Department of Defense installations and personnel dependent on TRICARE, the government-sponsored health insurance program for active-duty members, retirees, and their families.
Doctors, clinics, and specialized health care providers in the region report that they are no longer receiving timely compensation for services rendered to TRICARE beneficiaries.
Breitbart News and local outlets highlight the financial strain these delays are causing, particularly for small practices and clinics that rely heavily on steady reimbursements to sustain operations.

For providers who serve families with children who have developmental disorders or chronic medical needs, the stakes are particularly high.
TRICARE and Its Critical Role
TRICARE is the health care program designed to ensure that active, reserve, and retired military members, along with their families, have access to comprehensive medical coverage.
It encompasses a variety of benefits, including access to civilian providers, military treatment facilities, prescription coverage, and specialized care for chronic conditions or disabilities.
For military families living in San Antonio, TRICARE is not merely an insurance plan—it is a lifeline.
San Antonio is home to Joint Base San Antonio (JBSA), which encompasses four major military installations: Lackland Air Force Base, Randolph Air Force Base, Fort Sam Houston, and Camp Bullis.
Collectively, these facilities support tens of thousands of active-duty personnel, retirees, and their dependents, all of whom rely on TRICARE to cover their medical expenses.
The ongoing shutdown has created a ripple effect across these installations, leaving health care providers without reimbursement and families facing uncertainty about accessing care.
Financial Strain on Health Care Providers
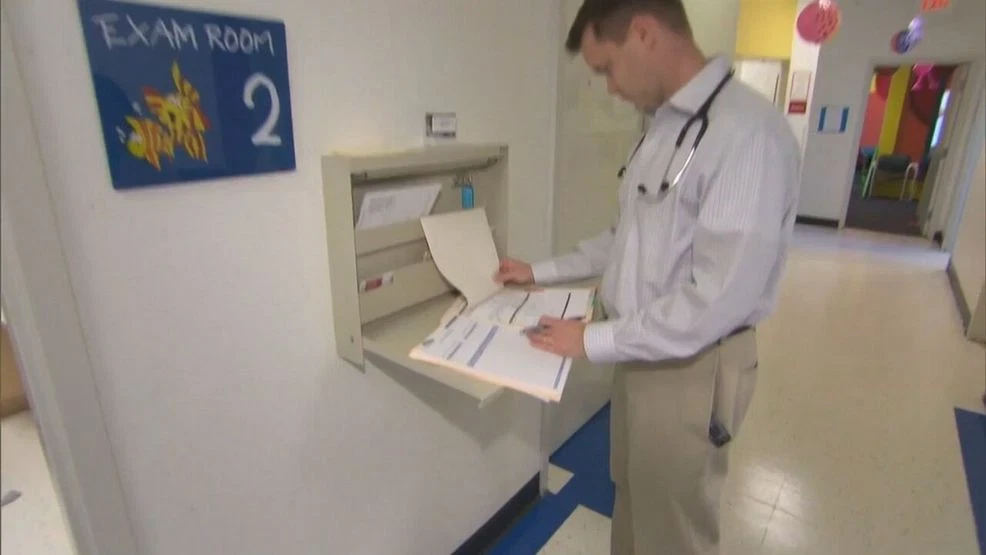
Local health care providers are reporting unprecedented strain as payments stall. Dr. Britt Sims, Executive Director of Integrated Behavior Solutions, a clinic serving children with developmental disorders, spoke candidly about the challenges.
“We can last a couple of weeks on what I have personally, but now, I’m done. I’m spent. If by some miracle, something happens, then I don’t know. We’ll keep fighting somehow,” she told News4SA.
Similarly, Dr. Gia Koehne, owner of the Blossom Center for Children, explained the immediate effects on her practice, which provides services for children diagnosed with autism.
“Because of all of this, everything is completely stalled and halted,” Koehne said. “We have a lot of families that need services, and we just don’t have the capacity to be able to do that, because we’re not getting paid.”
The stalling of reimbursements is not only a financial concern—it is a direct threat to continuity of care. Clinics providing therapy, behavioral health services, specialized pediatric care, and chronic condition management depend on predictable cash flow to maintain staff, pay rent, and secure necessary medical supplies.
Any interruption, even short-term, can jeopardize treatment schedules that military families rely upon.
Legislative Impasse Behind the Shutdown
The funding lapse stems from an ongoing budget impasse in Congress. Senate Democrats have prioritized extending Affordable Care Act subsidies as part of any potential deal to reopen the government.
Meanwhile, key appropriations necessary to fund TRICARE reimbursements remain stalled. Critics warn that the standoff not only risks disrupting care for military families nationwide but has particularly acute consequences in areas like San Antonio, where the density of Department of Defense installations amplifies the impact.
For military retirees, the uncertainty is especially troubling. Many retirees rely exclusively on TRICARE to cover medical costs, including prescription medications, routine care, and treatment for age-related conditions.
Without timely payments to providers, access to care can become sporadic, forcing retirees to delay treatments or seek alternative options that may be costly or inconvenient.
Human Stories from the Ground
The effects of the shutdown are felt most acutely by the families themselves. At Integrated Behavior Solutions, therapists and staff have seen an increase in anxiety among parents concerned about potential disruptions in their children’s care.

One mother, whose son receives weekly behavioral therapy, explained, “I don’t know how long this will last, and every day without therapy is a setback. It’s terrifying because we rely on these services for his progress.”
Similarly, at the Blossom Center for Children, parents of children with autism reported the strain of uncertainty. Many had structured routines around weekly sessions, which provide not only educational and therapeutic support but also a predictable environment essential for children with developmental challenges.
Delays in funding threaten to disrupt these schedules, potentially undoing months of progress and creating emotional stress for families.
Official Guidance and TRICARE’s Response
TRICARE has issued guidance acknowledging potential delays. Members are advised that they can continue to access care at military treatment facilities or through civilian providers, and standard out-of-pocket costs apply.
Prescription services at military pharmacies, retail network pharmacies, and home delivery are available; however, claims submitted on or after October 1, 2025, may not be processed until funding is restored.
The Defense Health Agency (DHA) is coordinating with TRICARE contractors to communicate with providers about anticipated delays in payment. In a memo, TRICARE emphasized:
“We understand this may cause concern and inconvenience, and we sincerely regret the disruption. We remain committed to resuming full operation as quickly as possible once appropriations are enacted.”
While this guidance reassures members about access to care, it does not alleviate the financial strain experienced by providers or the anxiety of families worried about potential interruptions.
The Trump Administration’s Interim Measures
To mitigate some immediate effects, the Trump administration announced measures to ensure that active-duty service members continue to receive pay despite the ongoing shutdown.
Officials indicated that unused funds originally allocated for research and development would be redirected to cover military payroll until government funding is restored.
While this guarantees income for troops, it does not directly resolve the challenges faced by civilian health care providers or military retirees dependent on TRICARE payments.
Providers continue to operate with uncertainty, balancing financial survival with the imperative to maintain care for some of the most vulnerable members of the military community.
As the shutdown stretched into its second week and beyond, San Antonio’s health care landscape began to feel the cumulative effects of delayed TRICARE payments. For civilian providers, the challenge was no longer just operational—it had become a question of sustainability.
Small practices that rely heavily on prompt reimbursement for salaries, rent, and medical supplies faced the real possibility of temporary closure. Clinics that had served military families for decades now struggled to maintain staffing, retain specialists, and deliver consistent care to patients with chronic conditions.
Local Government and Community Reactions
The city of San Antonio quickly mobilized local officials, veterans’ organizations, and nonprofit advocacy groups to assess the impact on both service providers and the families who rely on them.
City Council member Rebecca Martinez noted, “Military families in our community deserve reliable access to health care. The federal shutdown is creating uncertainty not only for active-duty members but for retirees and children with specialized medical needs.”
Veterans’ advocacy groups began organizing community forums to support affected families and coordinate temporary resources. Local hospitals, aware of the potential surge in emergency visits if routine care was delayed, started collaborating to provide guidance and extend appointments for critical cases.

While these efforts provided some relief, they could not fully replace the financial lifeline provided by TRICARE reimbursements.
Impact on Specialized Care
One of the most pressing concerns emerged among providers who care for children with developmental disorders, such as autism or cerebral palsy. Structured, consistent therapy is essential for maintaining progress, and disruptions can result in setbacks that require months to overcome.
Clinics such as Integrated Behavior Solutions and the Blossom Center for Children highlighted the dual challenges of maintaining services while managing financial shortfalls.
Parents voiced deep anxiety about the shutdown’s long-term effects. One mother shared, “Even a two-week gap in therapy can feel like lost months for my child. The uncertainty is heartbreaking, and we’re constantly worried about what will happen next.”
Moreover, clinics that provide mental health services to military families—who often face unique stressors related to deployments, relocation, and the challenges of military life—warned that delayed payments could exacerbate mental health issues. These services, essential for overall family wellness, are particularly vulnerable during funding lapses.
Economic Ripple Effects
The shutdown’s financial impact extends beyond individual clinics. Suppliers of medical equipment, pharmacies, and ancillary service providers also feel the strain.
Hospitals and clinics often maintain accounts receivable with expectations of timely government reimbursement. Delays can lead to cash flow shortages, forcing some suppliers to pause shipments or demand upfront payments.
This economic ripple effect can touch every facet of the local economy, from payroll for support staff to local businesses that serve military families.
In San Antonio, where military installations significantly influence the city’s economic ecosystem, a prolonged shutdown could result in temporary layoffs, reduced community spending, and an overall contraction in local business activity.
Federal and Policy Perspectives
At the federal level, policymakers expressed concern about the potential for long-term disruption in military family services. Congressional leaders acknowledged the urgency of restoring funding but remained divided over the broader budgetary issues causing the shutdown.
Some legislators emphasized that ensuring uninterrupted access to TRICARE and military health services should be a top priority.
TRICARE itself emphasized that while services could continue during the lapse, delayed reimbursements would persist until appropriations were restored. The Defense Health Agency worked with contractors to communicate proactively with providers, but the operational strain remained evident on the ground.
Experts in public health and military policy stressed the importance of contingency planning for future shutdowns.
Dr. Amanda Reynolds, a health policy analyst, noted, “This shutdown underscores the fragility of health care financing for military families. Even temporary disruptions can have cascading effects, from financial stress on providers to gaps in essential care for vulnerable populations.”
Stories of Resilience
Despite the challenges, stories of resilience began to emerge. Clinics and providers found creative ways to continue serving families, offering telehealth appointments, prioritizing urgent care, and pooling community resources to cover immediate needs.
Volunteers, retired medical professionals, and local nonprofits contributed time and expertise to prevent service interruptions.
The Logan family, who live near Fort Sam Houston, shared how their local pediatric clinic provided virtual consultations during the shutdown, ensuring that their children with ongoing medical needs were not left without guidance.
These adaptive strategies, while temporary, demonstrated the community’s capacity to rally in times of crisis.
Long-Term Lessons
The San Antonio experience highlights a broader lesson for communities across the United States: the reliance on federally funded health care programs for military families is immense, and even short-term interruptions can have significant consequences.
Policymakers and local leaders are calling for stronger contingency planning, including emergency funding mechanisms, to protect providers and beneficiaries during government funding lapses.
Economists also stress that prolonged shutdowns have downstream effects on local economies. Reduced consumer confidence, delayed payments to service providers, and interruptions in essential care can all contribute to economic contraction, even beyond the immediate federal funding gap.
Moving Forward: Restoring Stability
As lawmakers work toward a resolution, the focus remains on restoring normal operations and stabilizing care for military families. Proposed solutions include:
Emergency Appropriations: Allocating interim funding to cover TRICARE reimbursements and ensure continuity of care.
Expanded Communication: Improving transparency between the Defense Health Agency, TRICARE providers, and families to minimize uncertainty.
Community Partnerships: Leveraging local nonprofits, hospitals, and veteran organizations to provide temporary support during lapses.
Policy Reform: Exploring mechanisms to insulate military health services from political gridlock, ensuring uninterrupted funding even during broader government shutdowns.
Experts agree that these measures could mitigate future risks, helping protect both providers and military families.
Reflections from the Community
For families and providers in San Antonio, the shutdown serves as a reminder of the fragility of essential services and the importance of community solidarity. Parents continue to express gratitude for the dedication of health care professionals who persist despite financial uncertainty.
Providers report that the crisis has strengthened relationships with families, reinforcing the shared commitment to prioritize children’s health and well-being.
Military families, while anxious about immediate disruptions, are inspired by the resilience of providers who continue to deliver care in challenging circumstances.
One mother said, “Even in the middle of this shutdown, I’ve seen the dedication and compassion of these doctors and therapists. It reminds me that we are not alone.”
Conclusion: A Community United Amid Uncertainty
The San Antonio case underscores the essential role of TRICARE and other federally funded programs in supporting military families. The shutdown illustrates the vulnerability of these systems to political stalemates and highlights the real-world consequences of funding delays.
Yet, the response from health care providers, local government, and community organizations demonstrates the power of resilience, creativity, and shared commitment.
Clinics have adapted, volunteers have stepped in, and families continue to advocate for the care their loved ones deserve.
Ultimately, the shutdown is more than a policy debate—it is a reminder that real people, real families, and real communities depend on stable, uninterrupted access to health care.
The lessons learned from San Antonio can inform policy, community preparedness, and future responses, ensuring that military families across the nation are never left without the support and services they have earned through their service and sacrifice.